Digital Health Strategic Implementation Roadmap
This Digital Health Strategic Roadmap was published in July this year. I took a few hours over the weekend to review it. While I might like to see a little more emphasis on use of AI to drive more innovation it is fair to say the document does not lack for lots of ambition. The document also is clear on the resources and challenges associated with this proposed 7 year implementation effort. Having worked in the sector over the last 15 years (in private healthcare) I have had first hand experience of the challenges associated with the required levels of change.
Interestingly the outline budget requires IT spend to go from 2.2% of total healthcare spend to 4-6%. Given current pressures on healthcare spend this would most likely require additional funding – at east until we begin to see payback in terms of efficiency post implementation.
The Summary – Digital Health Strategic Roadmap
At summary level the Roadmap aims to integrate digital technologies into Ireland’s healthcare system, promoting a patient-centered, digitally enabled environment. This roadmap aligns with key frameworks, including the Department of Health’s “Digital for Care” framework, the Sláintecare Action Plan, and the Digital Ireland Framework. It emphasises six core principles:
- patient empowerment,
- enhancing workforce and workplace,
- enabling digitally connected care,
- using data-driven services,
- fostering a digital health ecosystem and innovation, and
- establishing secure digital foundations.
The roadmap outlines 48 strategic initiatives over seven years, focusing on improving access, efficiency, and quality of care. It seeks to empower patients by giving them greater access to information and enhancing the healthcare workforce’s digital capabilities. Key outcomes include seamless data sharing, better patient involvement in care, and enhanced decision-making through data and analytics.
The roadmap stresses significant investment in digital infrastructure and skills, collaboration across healthcare systems, and robust governance to support this transformation. The goal is to create a more resilient, efficient, and high-quality healthcare system, benefiting patients and healthcare professionals alike
My ‘top 5’ projects
The following five projects – of 48 in total, caught my immediate attention:
- Electronic Health Records (EHR) Deployment: This project focuses on developing a national EHR system that provides seamless integration of patient data across various healthcare settings. This includes creating business cases, establishing standards, and setting up a procurement framework to ensure the EHR system is interoperable and secure
- National Shared Care Record (NCSR): Aimed at integrating health information to provide a holistic view of patient care, this initiative seeks to establish a unified care record accessible to healthcare providers across the country. This will enhance care coordination and improve patient outcomes by ensuring all relevant health data is available to caregivers
- Integrated Community Case Management System (ICCMS): This project aims to implement a system that supports the management of complex care cases within the community setting. By enabling better data sharing and coordination among community healthcare providers, this system will improve patient care and reduce the need for hospital admissions
- Digital Front Door and Managed Health Content: This initiative involves creating a central digital platform to provide health information, access to services, and digital tools for self-management. It will act as the primary entry point for patients to engage with the health system, facilitating easier access to care and information
- Cybersecurity Enhancement Program: Following the cyberattack on the HSE, this project is designed to bolster the digital health system’s cybersecurity infrastructure. It aims to protect patient data and healthcare systems from future cyber threats by implementing robust security measures and continuous monitoring
Risks to the Implementation Roadmap
- Cybersecurity Threats: There is a significant risk of cyber attacks, as demonstrated by the 2021 ransomware attack on the HSE, which disrupted patient care and access to health records. To mitigate this, a dedicated cybersecurity program is proposed to enhance the cyber resilience of the health system
- Funding and Resource Allocation: The roadmap requires substantial and sustained investment, estimated to be between 4% and 6% of the overall healthcare expenditure annually. Securing this funding is critical for the development of infrastructure, digital tools, and workforce skills
- Change Management and Adoption: Successfully transitioning to a digital health system involves overcoming resistance to change within the workforce and ensuring that patients and healthcare professionals are adequately trained and supported. Effective change management and leadership are essential to facilitate this transformation
- Data Quality and Integration: Ensuring high-quality data and seamless interoperability across various healthcare systems is crucial. Poor data quality and fragmented data sources could hinder effective care delivery and decision-making
Other points of interest in the Digital Health Strategic Roadmap
EHR implementation
There are a range of ERP products already in place. Cerner (now Oracle Healthcare) is in the Maternity Hospitals, the National Labs and James’. The Children’s Hospital recently selected and is implemting Epic. Many of the other hospitals have developed and implemented other solutions over the years. On the private side MEDITECH seems to have the bulk of the market (Beacon, Mater Private, Bons and Blackrock Health).
Given the objective appears to be to have one patient recrod – sourcing data from both public and private – will be interesting to see how this unfolds in the next 2 years. With this in mind also to be noted that the private sector in general is not coding diagnosis and treatment (will this be a requirement in order to develop an effective patient record?) Who will provide the budget for this, if required?
Digital Maturity
Strategy includes an outline digital maturity assessment – this assessment is directy relevant to the abiility of the healthcare system to take on board the level of change associated with the listed 48 projects. If the objective, as it should be, is to improve digital maturity there may be a significant requirement for development/ training/ building of sustainable teams.
Artificial Intelligence
This is addressed in a number of places in the roadmap. In fairness digitalisation (and availability of digital data) is a prerequiste for deployment of AI. However I suspect there are lots of opportunities to front load some of the AI delivery – even leveraging what’s available digitally now.
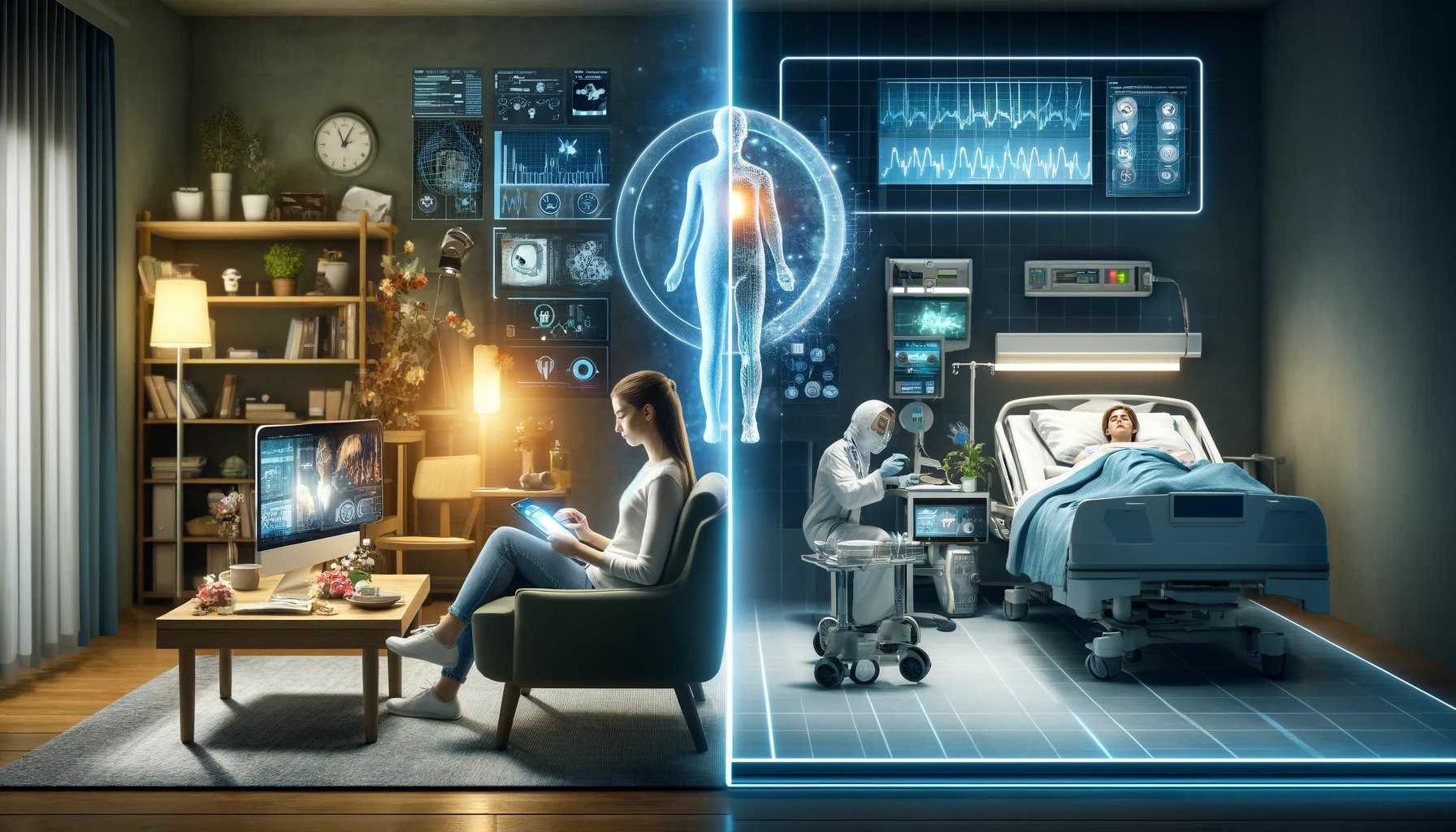
Shift Left, Stay Left
Great to see this called out in the roadmap – essential to move as much as possible out of acute care and back to community and/or home. Digital plays a key role in making this happen.
What are the next steps?
A roadmap without resources (cash, people, partners) is only a roadmap. Presumably now critical to approve funding to enable the healthcare digital transformation accelerate (and finalise the deliverables and timelines). Given pressures on staffing and resources critical to drive forward with this scope of work.